1. Psoriasis Vulgaris
This form is prevalent because it called psoriasis vulgaris. Named as well as lesions of plaque-type lesions are generally shaped plaque. Place predileksinya namely the scalp, scalp border with the face, extremities, especially the extensor ie knees, elbows and lumbosacral region.
 |
| Psoriasis Vulgaris |
2. Psoriasis guttate
Diameter abnormalities are usually less than 1 cm. Sudden onset and disseminated, is generally after Streptococcus infection in the upper respiratory tract after influenza or morbili especially in children and young adults. It also can occur after other infections both bacterial and viral.
 |
| Psoriasis Guttate |
3. Inversa Psoriasis (Psoriasis Flexural)
Psoriasis has a place in the flexor predilection to its name.
 |
| Psoriasis Flexura |
4. Psoriasis Exudative
This form is very rare. Usually abnormalities in psoriasis it in dry form, but in this type such as exudative dermatitis is acute.
5. Psoriasis Seborrhoeic
The clinical features of psoriasis seborrheic a combination of psoriasis and seborrheic dermatitis, which is usually dried squama be a bit oily and somewhat soft. Apart is a location commonly, also found in place seborrheic.
 |
| Psoriasis Seborrhoeic |
6. Psoriasis pustulosa
There are 2 opinions about psoriasis pustulosa, first considered as a separate disease, both regarded as a variant of psoriasis. There are 2 forms of psoriasis pustulosa namely:
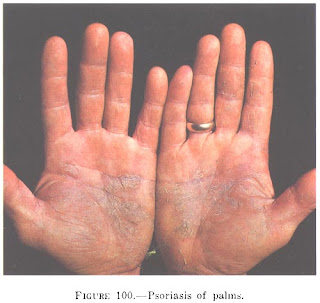
a. Pustulosa palmoplantar psoriasis (Barber)
Pustulosa palmoplantar psoriasis are chronic and residif, the palms of the hands or soles of the feet or both. Abnormalities of the skin in the form of small groups of sterile pustules and deep, over an erythematous skin, accompanied by itching.
 |
| Pustulosa palmoplantar psoriasis (Barber) |
b. Pustulosa Acute Generalized Psoriasis (Von Zumbusch)
Psoriasis pustulata acute generalized (von Zumbusch) can be caused by a variety of provocative factors, such as the most common drug for systemic corticosteroid discontinuation. Other drugs for example, penicillin and its derivatives, as well as other antibiotic Betalaktam, hidroklorokuin, potassium iodide, morphine, sulfapiridine, sulfonamide, codeine, Fenilbutason, and salicylates. Factors other than the drug is hypocalcemia, sunlight, alcohol, emotional stress, as well as bacterial and viral infections. This disease can occur in people who are or have got psoriasis. Can also appear in people who have never suffered from psoriasis. Symptoms initially are skin pain, hyperalgesia accompanied by general symptoms such as fever, malaise, nausea, anorexia. Plaque psoriasis who have been there more erythematous. After a few hours raised edematous and erythematous plaques much on normal skin. Within a few hours many pustules arise billion in these plaques. In a day-pustules pustules confluences lake of pus forming sized some cm great Pustule . Spongioform occurred due to migration of neutrophils into the Malpighian stratum, in which these neutrophil aggregate in between keratinocytes and degenerates. Thinning disorders such will continue and can be erythroderma. Laboratory tests showed leukocytosis, culture of pus from sterile pustules.
 |
| Pustulosa Acute Generalized Psoriasis (Von Zumbusch) |
7. Psoriatic erythroderma
Erythrodermic psoriasis can be caused by topical treatment that is too strong or widespread as the disease itself. Usually the lesions were typical for psoriasis not looked back since there is erythema and thick squama universal. Sometimes psoriasis lesions still loomed over erythematous and the skin is rising.
 |
| Psoriasis Erythrodrmic |











